Addison's Disease Explained: A Deep Dive Into Adrenal Health
Table of Contents
- Understanding Addison's Disease: The Foundations
- The Critical Role of Adrenal Hormones
- Recognizing the Signs: Symptoms of Addison's Disease
- Diagnosing Addison's Disease: The Medical Journey
- Treatment Approaches for Addison's Disease
- Distinguishing Addison's from Related Conditions
- The Mayo Clinic's Expertise in Adrenal Conditions
- Living with Addison's Disease: Management and Outlook
Understanding Addison's Disease: The Foundations
Addison's disease, medically known as primary adrenal insufficiency, is a rare disorder that occurs when the adrenal glands produce insufficient amounts of certain hormones. These small, triangular-shaped glands are perched atop each kidney, playing a pivotal role in the endocrine system. In Addison's disease, the primary issue lies within these glands themselves, meaning they are directly damaged and unable to function properly. This distinguishes it from secondary adrenal insufficiency, a related condition where the problem originates in the pituitary gland, which fails to produce enough adrenocorticotropic hormone (ACTH), a hormone that stimulates the adrenal glands. These conditions have different causes, highlighting the importance of accurate diagnosis to ensure appropriate treatment. Understanding the root cause of the adrenal dysfunction is the first critical step in managing the condition effectively. The most common cause of Addison's disease is an autoimmune response, where the body's immune system mistakenly attacks its own adrenal glands. This slow, progressive destruction leads to a gradual decline in hormone production. Less common causes include infections (such as tuberculosis), cancer, bleeding into the adrenal glands, or genetic defects. Regardless of the underlying cause, the consequence is a severe deficiency in vital hormones, which profoundly impacts various bodily functions. This foundational understanding sets the stage for comprehending the wide array of symptoms that can manifest in individuals with Addison's disease.The Critical Role of Adrenal Hormones
The adrenal glands are powerhouses of hormone production, specifically responsible for synthesizing cortisol and aldosterone. In Addison's disease, the adrenal glands make too little cortisol and, often, too little aldosterone. These hormones control important body functions, and their deficiency leads to the characteristic symptoms of the disease. * **Cortisol:** Often referred to as the "stress hormone," cortisol plays a multifaceted role in the body. It helps the body respond to stress, regulates metabolism (how the body uses food for energy), maintains blood pressure, reduces inflammation, and influences the immune system. A deficiency in cortisol can lead to profound fatigue, weakness, weight loss, low blood pressure, and a heightened susceptibility to infections. The body's ability to cope with even minor stressors is severely compromised without adequate cortisol. * **Aldosterone:** This hormone is crucial for regulating the body's balance of sodium and potassium, which in turn affects blood pressure and fluid balance. Too little aldosterone can lead to low blood pressure, dizziness, salt cravings, and an imbalance of electrolytes, which can be life-threatening if severe. The combined deficiency of these two critical hormones underscores the systemic impact of Addison's disease on overall health and well-being. Their proper balance is essential for maintaining homeostasis and ensuring the body's systems function harmoniously.Recognizing the Signs: Symptoms of Addison's Disease
The symptoms of Addison's disease often develop slowly over time, making early diagnosis challenging. They are usually non-specific at first, gradually worsening as the adrenal glands fail further. Recognizing these signs is crucial for prompt medical attention. Common symptoms include:- Chronic, worsening fatigue and muscle weakness
- Weight loss and decreased appetite
- Low blood pressure (hypotension), which can lead to dizziness or fainting
- Darkening of the skin (hyperpigmentation), especially in scars, skin folds, and pressure points like elbows and knees. This is due to increased ACTH, which also stimulates melanin production.
- Salt craving, due to the loss of sodium from the body
- Low blood sugar (hypoglycemia)
- Nausea, vomiting, diarrhea, or abdominal pain
- Muscle or joint pains
- Irritability or depression
- Loss of body hair or sexual dysfunction in women
| Symptom Category | Specific Manifestations |
|---|---|
| General | Chronic fatigue, muscle weakness, weight loss, decreased appetite |
| Cardiovascular | Low blood pressure, dizziness, fainting |
| Skin | Darkening of skin (hyperpigmentation) |
| Electrolyte/Fluid | Salt craving, dehydration, electrolyte imbalances |
| Gastrointestinal | Nausea, vomiting, diarrhea, abdominal pain |
| Metabolic | Low blood sugar |
| Musculoskeletal | Muscle or joint pains |
| Psychological | Irritability, depression |
- Sudden, severe pain in the legs, lower back, or abdomen
- Severe vomiting and diarrhea, leading to dehydration
- Profound weakness and lethargy
- Low blood pressure (hypotension) that can lead to shock
- Loss of consciousness
- High potassium and low sodium levels
Diagnosing Addison's Disease: The Medical Journey
Enfermedad de Addison diagnóstico: el diagnóstico implica los pasos que sigue tu equipo de atención médica para descubrir si tienes o no la enfermedad de Addison. Given the non-specific nature of early symptoms, diagnosing Addison's disease can be challenging and often requires a high degree of clinical suspicion. The diagnostic process typically involves a combination of physical examination, review of symptoms, and specialized laboratory tests designed to measure hormone levels and assess adrenal function. Key diagnostic steps include:- **Blood Tests:** These tests measure levels of sodium, potassium, cortisol, and ACTH. In Addison's disease, blood tests typically show low cortisol, high ACTH (as the pituitary tries to stimulate the failing adrenal glands), low sodium, and high potassium.
- **ACTH Stimulation Test:** This is the most definitive test for diagnosing Addison's disease. A synthetic form of ACTH is injected, and blood cortisol levels are measured before and 30 or 60 minutes after the injection. In healthy individuals, cortisol levels will rise significantly. In people with Addison's disease, the adrenal glands will produce little or no cortisol in response to the ACTH stimulation.
- **Insulin-Induced Hypoglycemia Test:** Less commonly used now, this test involves injecting insulin to lower blood sugar, which should stimulate cortisol and growth hormone production. It's used to assess the function of the pituitary gland and adrenal glands.
- **Imaging Tests:** While not directly diagnostic for Addison's disease itself, imaging such as a CT scan or MRI of the adrenal glands and pituitary gland may be performed to look for other causes of adrenal insufficiency, such as tumors or infections, or to assess the size and structure of the adrenal glands.
Treatment Approaches for Addison's Disease
Treatment addison's disease treatment involves taking medicines to correct the levels of steroid hormones that the body isn't making enough of. This is a lifelong therapy, as the adrenal glands cannot recover their function. The primary goal of treatment is to replace the deficient hormones, bringing the body's hormone levels back to normal and alleviating symptoms. The cornerstone of Addison's disease treatment is hormone replacement therapy, typically involving:- **Glucocorticoids (e.g., Hydrocortisone, Prednisone, Dexamethasone):** These medications replace cortisol. Hydrocortisone is often preferred because its action mimics the body's natural cortisol rhythm, with higher doses taken in the morning and lower doses in the afternoon or evening. The dosage must be carefully managed and adjusted, especially during times of stress, illness, or surgery, to prevent an Addisonian crisis.
- **Mineralocorticoids (e.g., Fludrocortisone):** This medication replaces aldosterone. It helps regulate sodium and potassium levels and maintain blood pressure. Dosage adjustments are made based on blood pressure, sodium and potassium levels, and the presence of symptoms like salt craving or dizziness.
Distinguishing Addison's from Related Conditions
The endocrine system is complex, and several conditions can present with symptoms that might overlap or be confused with Addison's disease. Understanding these distinctions is vital for accurate diagnosis and appropriate treatment. These conditions have different causes, even if they involve the same hormones.Adrenal Fatigue: Is It Real?
Adrenal fatigue is a term used to describe a group of symptoms that aren't specific, such as tiredness, trouble sleeping, and body aches, often attributed to chronic stress overwhelming the adrenal glands. However, it's important to note that it's not an official medical diagnosis recognized by mainstream medical organizations. While chronic stress can certainly impact health, the concept of "adrenal fatigue" as a distinct medical condition with specific diagnostic criteria is not supported by scientific evidence. Unlike Addison's disease, where there is a measurable, life-threatening deficiency of adrenal hormones, "adrenal fatigue" lacks objective diagnostic markers. This distinction is crucial to prevent misdiagnosis and ensure that individuals with genuine adrenal insufficiency receive proper medical care.Cushing Syndrome: The Opposite End of the Spectrum
Cushing syndrome happens when the body has too much of the hormone cortisol for a long time. This is essentially the opposite of Addison's disease, where cortisol levels are too low. This can result from the body making too much cortisol, often due to a tumor in the pituitary gland (Cushing's disease) or adrenal gland, or from taking high doses of corticosteroid medicines for conditions like asthma, arthritis, or lupus. Symptoms of Cushing syndrome include weight gain (especially in the face, neck, and trunk), thinning skin, easy bruising, high blood pressure, high blood sugar, and muscle weakness. Understanding the difference between these two conditions is fundamental, as one requires hormone replacement and the other requires reducing hormone levels or removing the source of excess production.Hashimoto's Disease: Another Autoimmune Connection
Hashimoto's disease is an autoimmune disorder affecting the thyroid gland, leading to hypothyroidism (underactive thyroid). While it directly affects the thyroid and not the adrenal glands, it's relevant in the context of Addison's disease because both are autoimmune conditions. Individuals with one autoimmune disorder have a higher risk of developing other autoimmune conditions. Therefore, a person diagnosed with Hashimoto's disease might also be screened for Addison's disease, and vice versa, as part of a comprehensive health assessment. This highlights the interconnectedness of the immune system and its potential impact on various endocrine glands.The Mayo Clinic's Expertise in Adrenal Conditions
When dealing with complex and rare conditions like Addison's disease, seeking care from highly experienced medical centers is paramount. Departments and specialties at institutions like the Mayo Clinic exemplify this expertise. The Mayo Clinic has one of the largest and most experienced practices in the United States, with campuses in Arizona, Florida, and Minnesota. Their integrated approach to patient care means that individuals with adrenal conditions benefit from a multidisciplinary team of endocrinologists, radiologists, pathologists, and surgeons who collaborate to provide comprehensive diagnosis and treatment. Their vast experience ensures that patients receive the most accurate diagnoses, even for challenging cases, and access to the latest treatment protocols and clinical trials. The Mayo Clinic's commitment to research and patient education also contributes significantly to advancing the understanding and management of adrenal disorders. This level of specialized care is invaluable for navigating the complexities of Addison's disease, from initial diagnosis to lifelong management and crisis prevention. Their authoritative stance in the medical community underscores the importance of relying on established and reputable sources for health information.Living with Addison's Disease: Management and Outlook
Living with Addison's disease is a lifelong journey that requires diligent self-management and regular medical supervision. With proper treatment, individuals with Addison's disease can lead full and active lives. The key to successful management lies in consistent adherence to medication schedules, understanding the nuances of stress dosing, and being prepared for potential crises. Patients are educated on the importance of:- **Consistent Medication:** Taking prescribed glucocorticoids and mineralocorticoids daily, exactly as directed. Missing doses or stopping medication can lead to an Addisonian crisis.
- **Stress Dosing:** Learning to increase medication doses during periods of physical stress (e.g., fever, flu, surgery, injury) to mimic the body's natural response to stress. This is critical in preventing a crisis.
- **Emergency Preparedness:** Carrying an emergency hydrocortisone injection kit and a medical alert identification (bracelet or card) at all times. This ensures that in an emergency, medical personnel are aware of the condition and can provide life-saving treatment.
- **Regular Monitoring:** Undergoing periodic blood tests and check-ups with an endocrinologist to monitor hormone levels and adjust medication as needed.
- **Hydration and Electrolyte Balance:** Paying attention to fluid intake and signs of electrolyte imbalance, especially during hot weather or illness.
- **Education and Support:** Actively learning about the condition and connecting with support groups or patient organizations. Knowledge empowers individuals to manage their health proactively.
Conclusion
Addison's Disease, or primary adrenal insufficiency, is a serious but manageable condition that arises from the adrenal glands' inability to produce sufficient cortisol and aldosterone. These hormones are vital for numerous bodily functions, and their deficiency can lead to a wide array of symptoms, culminating in the life-threatening Addisonian crisis if left untreated. Understanding the distinction between Addison's and related conditions like secondary adrenal insufficiency, Cushing syndrome, or even the unproven "adrenal fatigue" is crucial for accurate diagnosis. Lifelong hormone replacement therapy is the cornerstone of treatment, enabling individuals to lead healthy lives. The importance of expert medical care, such as that provided by institutions like the Mayo Clinic, cannot be overstated in navigating this complex condition. By adhering to medication, practicing stress dosing, and maintaining emergency preparedness, those with Addison's disease can effectively manage their health. If you or someone you know experiences symptoms suggestive of Addison's disease, do not hesitate to seek medical attention. Early diagnosis and consistent treatment are key to preventing severe complications and ensuring a good quality of life. Share this article to spread awareness about this important health condition, and consider exploring more resources from reputable medical organizations to deepen your understanding of endocrine health. Your proactive engagement in health education can make a significant difference.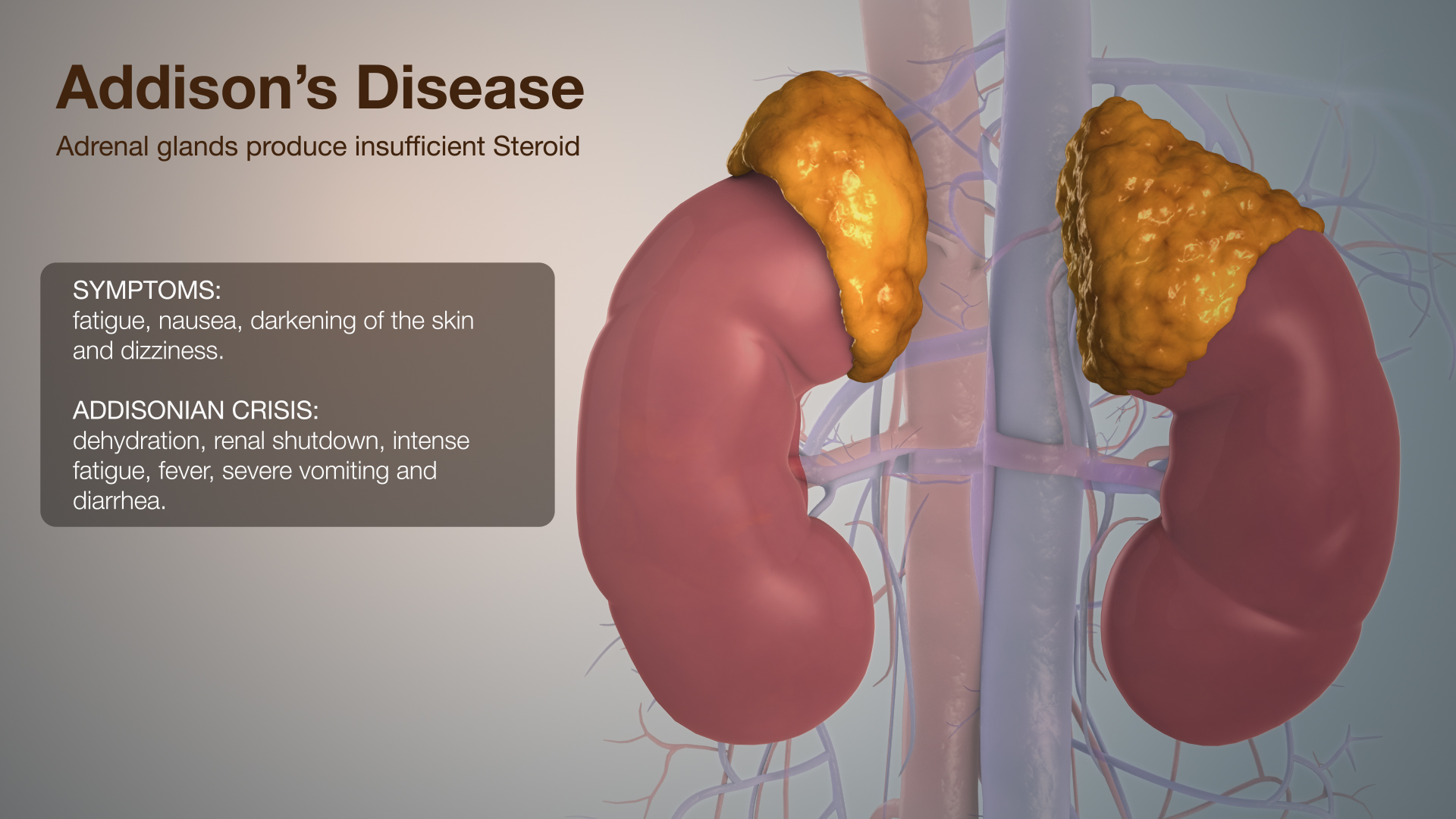
Addison's Disease Explained Using Medical Animation

Addison Rae Breaks Silence to Apologize for All Lives Matter Post

Addison Rae Wiki, Biography, Age, Boyfriend, Facts and More